A Review of Dr. Anthony Fauci’s Past Projections on the Wuhan Coronavirus
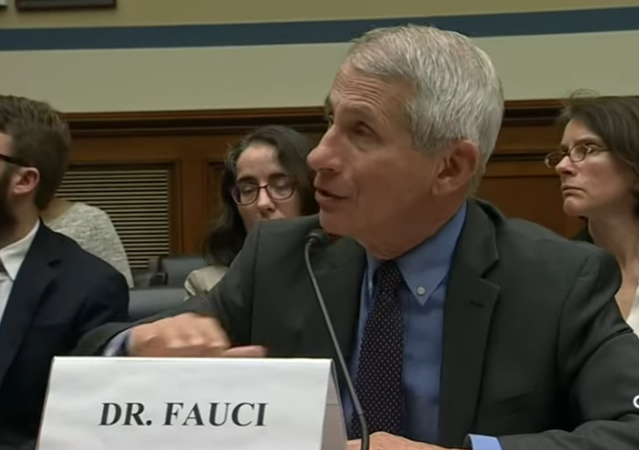
This Sunday morning, social media was abuzz with the news that Coronavirus Task Force member Dr. Anthony Fauci indicated that current models showed millions of Americans could have the Wuhan Coronavirus, and there could be as many as 100,000 deaths.
“Whenever the models come in, they give a worst-case scenario and a best-case scenario. Generally, the reality is somewhere in the middle. I’ve never seen a model of the diseases that I’ve dealt with where the worst case actually came out. They always overshoot,” Dr. Anthony Fauci, a key member of the White House’s coronavirus task force, told CNN’s Jake Tapper on “State of the Union.””I mean, looking at what we’re seeing now, you know, I would say between 100 and 200,000 (deaths). But I don’t want to be held to that,” he said, adding that the US is going to have “millions of cases.”
However, during Sunday afternoon’s Coronavirus Task Force briefing, Fauci clarified that he was relying on models, and the information used by those models included no intervention (which clearly is NOT occurring).
And he took the media to task for sensationalizing those numbers.
At this point, it is worthwhile taking a look at the previous predictions about the pandemic that Fauci made.
On February 28, 2020, the New England Journal of Medicine published online an article that lays out the opinions of leading medical scientists about the Wuhan Coronavirus and projects a possible future once the current wave of infections is over.
The analysis, Covid-19 – Navigating the Unknown (pdf.) – is co-authored by Fauci. He joined H. Clifford Lane (National Institute of Allergy and Infectious Disease (NIAID), Deputy Director for Clinical Research and Special Projects), and Robert R. Redfield (Director of the Centers for Disease Control and Prevention).
The relatively short article has information presented clearly and concisely. I would like to feature a few bits with supporting background information. The work provides historical background on the coronavirus research and maps out the battle strategy against the virus.
Many people have had already noted that it is difficult to gauge precisely how lethal the coronavirus is without knowing exactly how many people have the virus and recovered with few if any symptoms. The authors strongly suspect that the 1.4% mortality rate being reported is too high, with the real number being closer to severe strains of flu seen in previous pandemics (e.g, Asian Flu of 1957 and the Hong Kong Flu of 1968).
If one assumes that the number of asymptomatic or minimally symptomatic cases is several times as high as the number of reported cases, the case fatality rate may be considerably less than 1%. This suggests that the overall clinical consequences of Covid-19 may ultimately be more akin to those of a severe seasonal influenza (which has a case fatality rate of approximately 0.1%) or a pandemic influenza (similar to those in 1957 and 1968) rather than a disease similar to SARS or MERS, which have had case fatality rates of 9 to 10% and 36%, respectively.
There is good reason to believe the asymptomatic numbers are significant. Iceland is conducting mass testing, which includes people who have not experienced symptoms of COVID-19.
This testing concludes half of the carriers show no symptoms. Additionally, the majority of those tested who indicated they had symptoms (e.g., headache, fever, dry cough) experienced very mild symptoms.
While Iceland has only 218 confirmed cases among its tiny population, its testing program has produced crucial data about the coronavirus – that half of those who were tested positive have no coronavirus symptoms….“Early results from deCode Genetics indicate that a low proportion of the general population has contracted the virus and that about half of those who tested positive are non-symptomatic,” Thorolfur Guðnason, Iceland’s chief epidemiologist, was quoted as saying BuzzFeed News. “The other half displays very moderate cold-like symptoms.”
The difference between the flu and COVID-19 is that all of us have had influenza at some time. Therefore, an older adult may have antibodies to a flu strain to which they are exposed and can overcome the infection.
This is not the case for the Wuhan Coronavirus. Nobody had ever been infected with it before Patient Zero in China. Therefore, the older population is being struck because their immune systems are not as robust as younger patients, and has no way to adapt and fight this new pathogen.
A study of 425 patients from the Wuhan area bears out this projection.
The median age of the patients was 59 years, with higher morbidity and mortality among the elderly and among those with coexisting conditions (similar to the situation with influenza); 56% of the patients were male. Of note, there were no cases in children younger than 15 years of age. Either children are less likely to become infected, which would have important epidemiologic implications, or their symptoms were so mild that their infection escaped detection, which has implications for the size of the denominator of total community infections.
Fauci and his co-authors also reviewed the timing of the onset of the disease to the need for an infected person to be hospitalized.
For example, Li et al. report a mean interval of 9.1 to 12.5 days between the onset of illness and hospitalization. This finding of a delay in the progression to serious disease may be telling us something important about the pathogenesis of this new virus and may provide a unique window of opportunity for intervention.
The 15-days Guidelines allowed the nation to prepare to get the equipment and resources needed in-place before a wave of hospitalizations would be required. The 15-days also provided time to garner information possible treatment options for those experiencing symptoms. These include lopinavir-ritonavir, interferon-1β, the RNA polymerase inhibitor remdesivir, chloroquine, a variety of traditional Chinese medicine products, and intravenous hyperimmune globulin from recovered patients.
Based on Task Force briefing discussions with Fauci and fellow member Dr. Deborah Birx, it appears that the team projects that the coronavirus will disappear during the summer, and return in the fall. They are working with the President and the rest of his team to expedite testing, find and produce vaccines, and identify effective treatments while keeping the mortality rate as low as can be achieved in this first wave of infections.
It is critical to note that the models used provide a range of possible outcomes. A good example, and one which comes from The Institute for Health Metrics and Evaluation (IHME, an independent population health research center at the University of Washington Medicine). As we hit the date of April 30th, it will be interesting to see how accurate the range is, especially in light of the rapidly expanding treatment and drug options.
If the curve flattens to around 33,000 deaths, then that is approximately the same as a moderately bad flu year, and far short of the 100,000 the media was presenting this weekend.
President Donald Trump is working hard to reduce the number to as low as can be achieved, based on the advice of Fauci and other team members. They may have access to additional information that indicates the extension of guidelines to the end of April is warranted.
Fauci and his team continue to gather data, and adjustments will be made in the models as speculation is replaced by hard information and results. For now, it appears that Fauci and his team’s original roadmap for the pandemic was good.
CLICK HERE FOR FULL VERSION OF THIS STORY